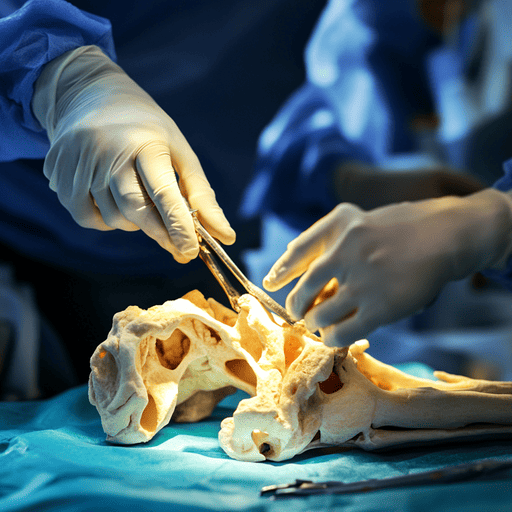
Soft tissue allografts are a cornerstone of reconstructive surgery, sports medicine, and orthopedic care. These grafts, derived from donated human tissue, are used to repair or replace damaged tendons, ligaments, fascia, and other soft tissues. By avoiding the need to harvest tissue from the patient’s own body, they reduce surgical complexity, recovery time, and morbidity. Their versatility makes them indispensable in treating injuries like torn ligaments, rotator cuff tears, and chronic wounds.
Soft tissue allografts are processed from donated tissues and categorized based on their application:
Tendon allografts: Used to repair torn tendons (e.g., Achilles tendon, rotator cuff).
Ligament allografts: Commonly used in ACL (anterior cruciate ligament) reconstruction.
Fascia lata allografts: Durable connective tissue used in hernia repairs or pelvic floor reconstruction.
Meniscus allografts: Replace damaged knee meniscus to restore joint function.
Learn more about tissue types: American Association of Tissue Banks (AATB).
Soft tissue allografts are indicated for:
Sports injuries: ACL tears, rotator cuff tears, or Achilles tendon ruptures.
Chronic wounds: Repairing tissue loss in diabetic ulcers or burns.
Reconstructive surgery: Restoring abdominal walls (hernia repair) or breast reconstruction post-mastectomy.
Orthopedic repair: Augmenting weak tissues in joint stabilization surgeries.
Clinical applications: Arthroscopy Journal.
No donor-site morbidity: Eliminates pain and complications from autograft harvesting.
Customizability: Available in various sizes and shapes to match patient anatomy.
Reduced surgery time: Pre-processed grafts streamline procedures.
Lower infection risk: Stringent sterilization protocols ensure safety.
Read about benefits: OrthoInfo (AAOS).
Safety is ensured through:
Donor screening: Rigorous medical history checks and infectious disease testing (e.g., HIV, hepatitis).
Tissue processing: Gamma irradiation or chemical sterilization to eliminate pathogens.
Regulatory compliance: FDA guidelines and AATB standards govern tissue banks.
Studies show high success rates, with 85–90% patient satisfaction in ACL reconstruction using allografts (Prodromos et al., 2020).

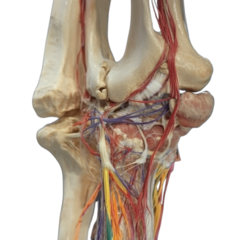
Soft tissue allografts undergo a process called ligamentization, where the donor tissue is gradually remodeled by the host’s cells. Key factors for success include:
Revascularization: New blood vessels grow into the graft.
Collagen alignment: The graft’s collagen fibers reorganize to mimic natural tissue.
Cellular repopulation: Host cells replace donor cells over 12–24 months.
Explore integration mechanisms: Journal of Orthopaedic Research.
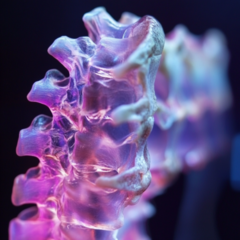
Recent advancements focus on enhancing graft performance:
Bioenhanced allografts: Grafts infused with growth factors (e.g., PRP, BMPs) to accelerate healing.
3D-printed scaffolds: Custom-designed matrices to guide tissue regeneration.
Stem cell integration: Combining allografts with mesenchymal stem cells to improve outcomes.
Minimally invasive techniques: Arthroscopic delivery of allografts for faster recovery.
Soft tissue allografts are a transformative solution for repairing complex injuries and restoring mobility. Their safety, versatility, and evolving innovations make them a gold standard in reconstructive and sports medicine. As research advances, these grafts will continue to bridge the gap between injury and full functional recovery.
Types of soft tissue grafts: NIH National Library of Medicine.
Patient success stories: Mayo Clinic.
Surgeon guidelines: Arthroscopy Association of North America.
We offer soft tissue allografts, with and without bone block, for various reconstruction and reinforcement procedures. All soft tissue allografts are terminally sterilized with low dose, low temperature irradiation to maintain biomechanical integrity of the tissue, while achieving a sterility assurance level (SAL) of 10-6










These cookies are necessary for the website to function and cannot be switched off in our systems. They are usually only set in response to actions made by you which amount to a request for services, such as setting your privacy preferences, logging in or filling in forms. You can set your browser to block or alert you about these cookies, but some parts of the site will not then work.
These cookies help us understand and improve the use and performance of our services including what links visitors clicked on the most, and how they interact with the various areas and features on our website and apps.