Wound Allografts: Accelerating Healing in Complex Wounds
Introduction
Wound allografts are advanced biological materials derived from donated human tissue, designed to promote healing in chronic or complex wounds that fail to respond to conventional therapies. These grafts provide a scaffold for tissue regeneration, reduce infection risks, and accelerate recovery in conditions like diabetic ulcers, burns, and surgical wounds. By leveraging the natural properties of donor tissue, wound allografts bridge the gap between impaired healing and functional recovery.
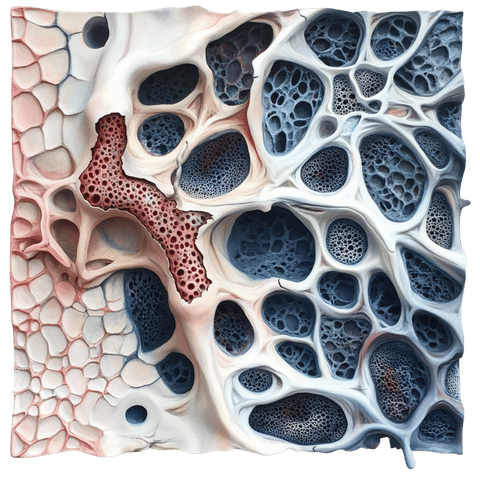
Definition and Types
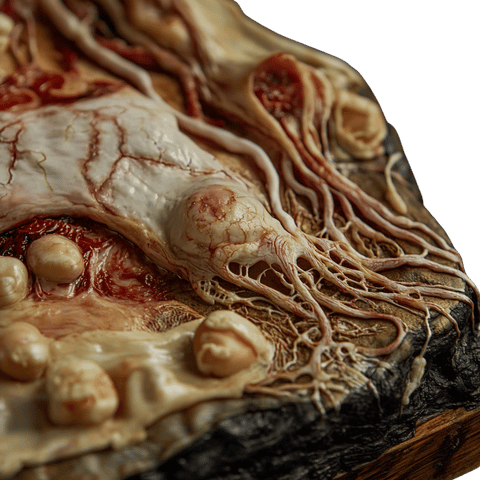
Wound allografts are processed to retain bioactive components that stimulate healing. Common types include:
Amniotic membrane allografts: Rich in growth factors and anti-inflammatory proteins, ideal for ocular and burn wounds.
Dermal allografts: Decellularized skin matrices that support new tissue growth in chronic ulcers.
Placental allografts: Contain collagen, hyaluronic acid, and cytokines to enhance wound closure.
Cellular allografts: Include living cells (e.g., fibroblasts) to actively repair damaged tissue.
Learn about graft types: American Association of Tissue Banks (AATB).
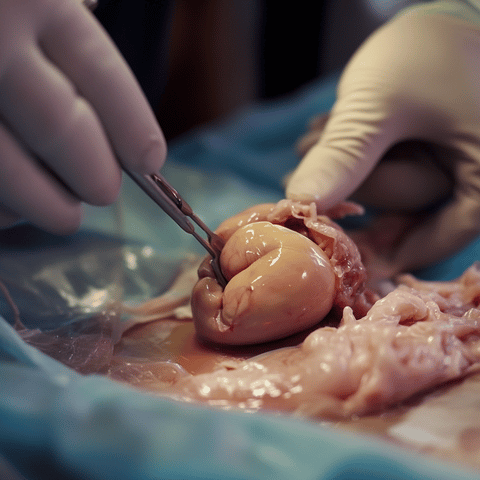
Indications for Use
Wound allografts are used to treat:
Diabetic foot ulcers: Stubborn wounds with high infection risks.
Burn injuries: Promote re-epithelialization in partial-thickness burns.
Venous leg ulcers: Improve healing in patients with poor circulation.
Surgical wounds: Aid recovery in non-healing post-operative sites.
Pressure ulcers: Prevent complications in bedridden patients.
Clinical guidelines: Wound Healing Society.
Advantages
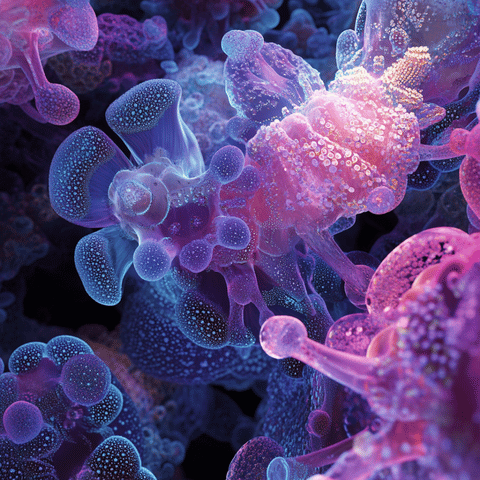
Enhanced healing: Bioactive components (e.g., growth factors) stimulate cell migration and angiogenesis.
Infection control: Antimicrobial properties reduce bacterial colonization.
No donor-site morbidity: Avoids secondary wounds from autograft harvesting.
Versatility: Adaptable to irregular wound shapes and sizes.
Read about efficacy: NIH National Institute of Diabetes and Digestive and Kidney Diseases.
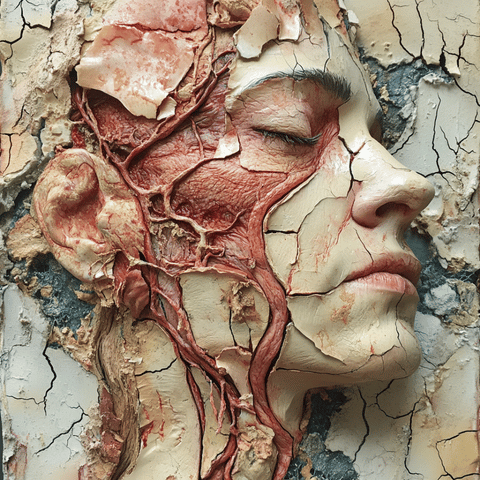
Safety and Efficacy
Safety protocols include:
Donor screening: Tests for HIV, hepatitis, and other pathogens.
Decellularization: Removes donor cells to minimize immune rejection.
Lyophilization: Freeze-drying preserves graft integrity without chemicals.
Studies report 70–80% healing rates in diabetic ulcers treated with amniotic allografts (Marston et al., 2021).

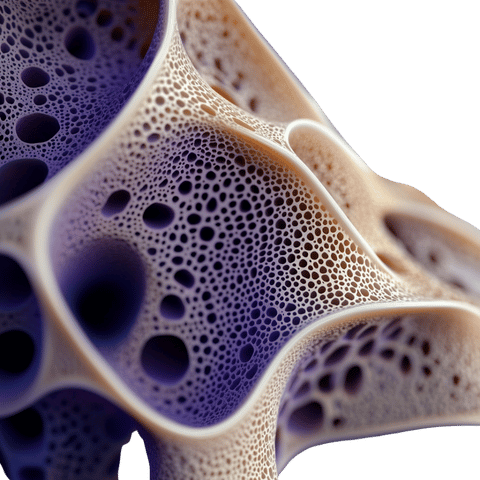
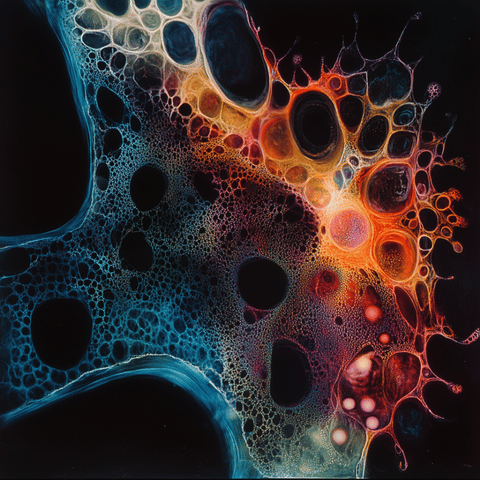
Biological Integration
Wound allografts work through:
Revascularization: New blood vessels form within the graft.
Cell recruitment: Host fibroblasts and keratinocytes migrate into the graft.
Extracellular matrix (ECM) remodeling: Donor collagen integrates with host tissue.
Explore mechanisms: Journal of Wound Care.
Research and Innovations
Recent breakthroughs include:
Cellular allografts: Genetically modified fibroblasts to secrete growth factors (e.g., PDGF).
Bioengineered matrices: 3D-printed scaffolds infused with stem cells.
Antimicrobial allografts: Grafts coated with silver nanoparticles or antibiotics.
Smart dressings: Allografts combined with sensors to monitor healing progress.
Cutting-edge research: Science Translational Medicine.
Conclusion
Wound allografts are revolutionizing the management of complex wounds, offering hope to patients with limited healing options. Their ability to reduce infection risks, accelerate recovery, and adapt to diverse wound types makes them indispensable in modern wound care. As research advances, these grafts will continue to push the boundaries of regenerative medicine.
Explore More
Types of wound allografts: NIH National Library of Medicine.
Patient outcomes: Mayo Clinic Wound Care.
Clinical trials: ClinicalTrials.gov.
